New Born Life Support
“85% breathe spontaneously
10% respond to simple stimulation
5% need inflation breaths
0.1% require compressions
0.05% ever receive adrenaline”
Newborn Life Support: Staying and Playing When It Matters
Neonatal Life Support (NLS) isn’t something most of us do often, but when it’s needed, it’s one of the most high-stakes situations in medicine. The vast majority of babies arrive crying and breathing within seconds of delivery, but a very small proportion need help. That’s where being prepared, understanding the physiology, and following the algorithm really counts.
Culture Shift: Stop the Scoop and Run
One of the big takeaways is cultural. In the ambulance service, many of us have absorbed the mindset of “get them to a grown-up.” That’s understandable — neonatal arrests are rare, and hospitals feel safer. But the reality is, scooping and running can kill a salvageable baby.
The right thing to do is to stay, follow the algorithm, and deliver the interventions that matter most: warming, airway management, and ventilation. The “grown-ups” in this situation are actually us.
Why Do Babies Collapse?
When resuscitation is needed, it’s often due to one of three categories of problems:
Maternal: hypertension, anaemia, shock, sepsis
Placental/cord: abruption, cord prolapse, haemorrhage
Neonatal: congenital airway or cardiac issues, sepsis, hypovolemia, drug exposure
Sometimes the issue is simply that the transition process stalls — fluid-filled lungs, delayed circulation changes, or inadequate initial breathing effort.
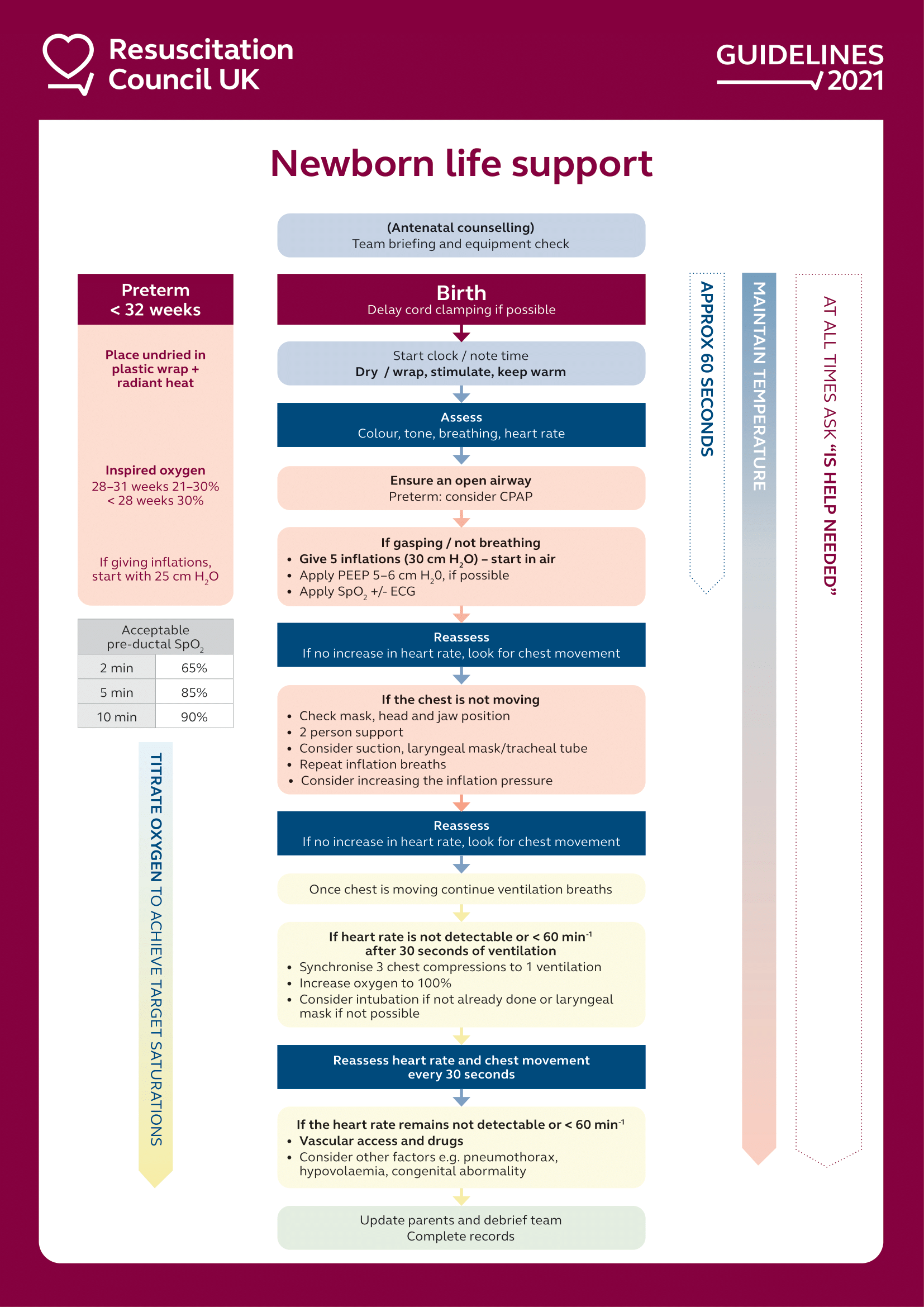
Image left: Credit JRCALC 2025 - NLS decision aid
The Numbers That Reassure
It’s worth repeating: only a very small minority of neonates need full NLS.
85% breathe spontaneously
10% respond to simple stimulation
5% need inflation breaths
0.1% require compressions
0.05% ever receive adrenaline
That’s why we follow the algorithm. It’s not about improvising under stress; it’s about calmly walking through the steps that are proven to work, even if we only use them once in a career.
When Do We Intervene?
The key time frame to remember is 22 weeks gestation. At 22 weeks and beyond, resuscitation is appropriate if needed. Below this threshold, the birth isn’t considered viable, and our role is to provide comfort care.
NLS applies during the first 24 hours of life, when the problem is usually a failure to transition from intrauterine to extrauterine physiology. After 24 hours, if a baby collapses, the cause is much more likely to be something separate (like sepsis or a congenital problem), and paediatric ALS (PALS) is the algorithm to follow.
What Does “Transition” Mean?
Before birth, babies don’t use their lungs for gas exchange. Oxygen arrives via the placenta, and blood bypasses the lungs through two key shortcuts:
The foramen ovale, a flap between the atria that lets blood cross from right to left.
The ductus arteriosus, a vessel shunting blood from the pulmonary artery straight into the aorta.
At birth, lung inflation lowers pulmonary resistance, blood flow shifts, and these shunts close. If this process doesn’t happen smoothly, babies can crash quickly. That’s why our very first job is to inflate the lungs — because ventilation drives that physiological switch.
And remember: when you check oxygen saturations, the right hand is the right hand. Pre-ductal sats (taken before blood crosses the ductus arteriosus) tell you the true picture of oxygenation.
First Assessments
Every assessment boils down to colour, tone, breathing, and heart rate.
About 85% of babies start breathing within 30 seconds of birth.
Another 10% respond to stimulation and drying.
Only 5% need inflation breaths.
Just 0.1% progress to compressions, and a vanishingly small number ever need adrenaline.
That’s encouraging: most of the time, simple steps are enough. But because these events are so rare, we absolutely have to know the algorithm cold.
Ventilation, Ventilation, Ventilation
If there’s one thing to tattoo on your brain about NLS, it’s this: ventilation is the cornerstone. The first few breaths should be slow, steady inflation breaths to recruit those fluid-filled lungs and help force fluid into the tissues. After that, you continue with normal ventilation, watching for chest rise.
No chest movement? Stop, troubleshoot. Mouth opening, mask seal, airway adjuncts — it’s usually something simple. The circular masks designed for neonates often give a better seal than the triangular ones many of us are used to.
Preparation: Half the Battle
By the time you’re in the middle of resuscitation, it’s too late to be scrambling for kit. Preparing a resuscitation area is one of the most powerful steps you can take. Essentials include:
Two towels (one for drying, one for wrapping)
A radiant warmer or transwarmer
Neonatal BVM and airway adjuncts
Suction with a thin catheter, tested and ready
Oxygen under the table (not pre-attached)
Stethoscope
A timer, phone, or clock for keeping track
And don’t forget an aide-memoir. No one is “too experienced” to benefit from having the algorithm in front of them.
The Cold Truth
If there’s one preventable killer we underestimate, it’s hypothermia. Babies lose heat fast: thin skin, large surface area-to-volume ratio, limited energy reserves. Mortality rises with every degree they lose — one study showed a 28% increase per degree below normal.
The fix?
Crank up the heating until you’re uncomfortably hot.
Dry thoroughly and wrap in a warm towel, replacing any that get damp.
Put a hat on — a huge proportion of heat is lost via the head.
Use transwarmers or radiant heaters when available.
For very premature babies (<32 weeks), skip drying and place them straight into plastic wrap under radiant heat.
If mum and baby are stable, skin-to-skin contact is another excellent way to preserve warmth — and delay clamping the cord if possible. Early clamping instantly reduces venous return to the baby’s heart by up to 50%, making the transition harder.
Final Thoughts
NLS is rare, stressful, and deeply emotional — but it’s also one of the most powerful things we can do for our patients. The key themes are simple:
Be prepared.
Keep the baby warm.
Focus on ventilation.
Don’t scoop and run.
Know the algorithm, and practise it.
Because when the moment comes, it’s not about heroics — it’s about following the basics, step by step, and giving that baby the best chance at life.
Key Takeaways
NLS starts at 22 weeks gestation and applies during the first 24 hours of life.
Ventilation is everything — inflation breaths followed by visible chest rise.
Prepare your resuscitation space: towels, heat, suction, oxygen, airway kit.
Hypothermia kills — keep babies warm from the start.
Don’t just scoop and run: effective care happens before transport.
Most neonates respond to minimal interventions, but when they don’t, algorithms guide us through.
Remember, clinicians are responsible for their own practice. These podcasts are produced for informative purposes and should not be considered solely sufficient to adjust practice. We provide lots of learning resources, so don’t just take our word for it…navigate to these and reflect on this topic further. See "The Legal Bit" for more info.
If you’ve got any comments on the article or podcast, please let us know using our Contact page, comment below or talk to us on Twitter!
Alternatively, you can come and chat with us about it on our Facebook group Parameducate.
If you like the podcast please leave us a review on the App store as it really helps boost our visibility so others can find our content, remember to tune in next month for our next General BroadCAST and don’t forget that you can check out our Archive for more free CPD!