Lower Back Pain
Lower Back Pain is a common presentation in prehospital care and it is estimated that 60-80% of the population have had back pain at some time during their life. Of these approximately 5-10% will have a degree of chronic back pain lasting for long periods. As a result ambulance clinicians will see those with acute back pain but also many with an exacerbations of their chronic pain.
The majority of lower back pain presentations are not serious, do not require imaging and can be managed safely in the community. However a small proportion can present with significant pathology and require emergent investigation, referral and management. Failure to recognise these significant presentations can have serious consequence for both the patient and clinician, as this can be a highly litigious clinical error if assessment was not performed adequately.
It is therefore essential that paramedics workup these patients thoroughly and document their findings accurately. In this episode of the podcast we will be discussing the assessment of patients presenting with lower back pain, the red flag symptoms and conditions that require referral and how to manage those patients who do not require hospital admission.
Anatomy and Physiology-
As we discussed in the podcast, A+P is really tricky to do justice in audio form. Additionally, we would only be repeating in text here, what could otherwise be explained far better in video form. Below are some really useful videos to help you get to grips with the structures we’re going to discuss later on in the article.
Low back pain is a common presentation to both primary care and emergency departments. As a service that works within this spectrum, ambulance clinicians will as a result, also see a high volume of these presentations. In fact within the UK 60-80% of people have reported lower back pain at some point in their lives [1]. In the main, most cases are non-specific and not serious [2]. However, all require a thorough workup.
Lower back pain is more prevalent in those who work in jobs that involve manual work due to lifting, bending, straining duties and also those with a high BMI, low socioeconomic class and patients with underlying mental health problems who often have worse recovery rates.
History Taking -
Enquire about the patients pain:
Site -
ask about exact location of the pain – is it, in fact, lower pain, be aware of thoracic level pain as a red flag (outside the scope of this article). Is it in the back of or does it arise from another structure e.g. genitourinary, hip, abdomen or lung (basal pneumonia can be a cause of back pain). Lower back pain can often be “refered” pain from another structure with a common nerve route [4] and this can be tricky to investigate, another reason we must have a structured and detailed assessment.
Onset -
When did the pain start? what was the patient doing at the time? Was there a causative event? Was it caused by trauma?
Did they wake up with the pain or woken up by it? This could be a cause for concern as something more sinister
Character –
Ask them to describe the pain? Ripping or tearing pain is worrying for aortic aneurysm dissection or rupture. Has the patient had pain like this before?
Radiation –
Does the pain go anywhere else? Pain radiating into the groin from the flank could be renal colic. Pain radiating from/ to the abdomen back has a range of sinister pathologies such as ruptured viscus, ischemic bowel or aortic pathology. Shooting pain down a leg could indicate radiculopathy. Be aware pain in the groin/ buttocks or legs can also be indicative of aortic pathology – in those over 50 with evidence of shock or collapse plus these symptoms think aorta until proven otherwise [3]
Associated Symptoms –
Sensory disturbance, motor disturbance, urinary retention/ incontinence or other new urinary sensation problems could indicate cauda equina syndrome (CES) or cord compression. Ask about fever/ chills/ flu like symptoms found in both acute pyelonephritis or vertebral infection/ vertebral discitis. Weight Loss/ night sweats – malignancy. Muscle spasms – trauma or soft tissue injury. Enquire about urinary symptoms such as incontinence or retention for Cauda Equina Syndrome (CES) or urgency, frequency, dysuria that in UTI.
Timing –
Duration – Minutes/ hours/days/ weeks/ months. How does it change over this time? Is the pain constant or is it fluctuating. Is the pain eased with rest or is there no change. Does the pain wake the patient at night?
Exacerbating / Relieving Factors –
Does anything make the pain better or worse. Worse at night could indicate ankylosing spondylitis or malignancy.
Severity –
Get a pain score from your patient. Ensure this is used properly and as originally designed. Pain scores are useful not only for you as a clinician to understand the patient’s subjective experience, but also to assess the effectivness of your analgesic regiment.
Severity should be considered holistically and its affect on the patients functional ability should also be commented on.
Ideas concerns and expectations:
Establish your patients Ideas, concerns and expectations early as this will help with agreed care plans. Many patients may worry and ask for imaging such as x ray or MRI scan, in patients who have no red flags that concern us according to NICE guidelines, imaging should not be offered [5] We therefore have a responsibility to explain this to patients and reassure them. Many patients simply want their pain controlled. We are in a unique place to offer this immediately along with onward advice and primary care referral for managing this in the forthcoming period.
Past Medical / Surgical History –
Previous back pain treatments – Physiotherapy, analgesia, steroid injections, spinal surgeries
Osteoporosis – increased risk of fracture
Trauma – Past traumas that have caused long standing back problems or recent trauma increases chances of muscular pain but also fracture. Be wary of the elderly even with low MOI trauma… this is one patient where it might be worth imaging.
Malignancy – consider metastases to the spine and pathological fractures. New or worsening back pain in the presence of another primary cancer should be a red flag and warrants referral for further assessment either via the GP urgently or hospital if emergency. Cancers that originate in the lung, breast, kidney, GI tract, Prostate or lymphomas and melanomas are all associated with a high risk of spinal mets [6]
Cardiovascular Disease/ Hypertension – increased AAA pathology risk.
Recent Infections/ Immunosuppression/IVDU – Risk of vertebral infection.
Depression - Indicative of worse recovery due to potentially poor engagment with physio. May need more support to aid recovery. [7]
Drug History –
Analgesia taken for the pain so far? – should be avoiding opiates in long term treatment however many patients still on these longstanding in high doses.
Benzodiazepines are falling out of favour but still often prescribed. Can theoretically help muscular spasm.
Gabapentin/ Pregabalin for chronic pain or nerve pain.
Corticosteroids – increased risk of vertebral infection if long term users.
Over the counter medicines – be aware of the patient accidently overdosing due to pain e.g. taking co-codamol 8/500mg and Paracetamol 1g at the same time. If you find this refer to ED for Paracetamol levels and overdose management.
Allergies – Always must be documented.
Social History -
Smoking – Increased risk of CVD and associated problems
Alcohol – Is the patient using alcohol for pain control or due to poor coping strategies with chronic pain. Increased risk of Pancreatitis which can radiate to the back (more likely thoracic level)
Recreational Drug Use – IVDU has an increased risk of vertebral infections such as Osteomyelitis/ Discitis/ Epidural abscess.
Occupation- What does their job entail – lifting, bending, repetitive movements, driving or sitting for prolonged periods. Is the patient currently able to do their job?
Stress – emotional stress can be high with those with back pain.
Activities of Daily Living – Are they coping with their home life, do they need support?
Examination -
As always if your patient is presenting very unwell or shocked, start with an A-E assessment and manage life threats. Otherwise: The examination should contain a comprehensive musculoskeletal (MSK) assessment as part of the process which should include a lower limb neurological examination integrated into it. Brief cardiorespiratory and abdominal assessments are also indicated to exclude other pathologies.
Cardiorespiratory –
Pulses including radial, brachial and femoral. Look for colour in the limbs, mottling/ pallor/ discolouration and pulse deficits can be indicative of aortic pathology [3]
BP – HTN is a risk factor for aortic disease. Be wary of common misconceptions often taught to paramedics that bilateral BP differences indicate AAA rupture and that if the bilateral BPs are the same this excludes AAA… this is a dangerous myth. Bilateral BP differences will only present in those patients with dissection at higher points within the thoracic aorta and not the abdominal aorta and even in those thoracic disections this has low clinical predictive value in isolation.[8]
Listen to the lungs and look for signs of respiratory infection e.g. fever, cough, SOB. Basal pneumonia may present with back pain.
Abdominal –
Look for signs of intra-abdominal pathology that may be masquerading as back pain e.g. AAA, ruptured viscus, ischemic bowel etc.
Palpation/ percussion of the bladder may indicate retention a symptom of late CES. [9]
Musculoskeletal – [10]
Gait – Can the patient walk, if so does the pain restrict this. If they can’t walk establish why, are they restricted due to pain or is there weakness or sensory changes in the lower limbs. If restricted by pain, consider administering pain control and then re-evaluating. Look for other signs of weakness e.g. foot drop.
Look -
Posture - lordosis
Deformity
Rashes e.g. shingles
Scars/ wasting
Bruising/ Wounds – trauma.
Feel -
Spinal/ bony tenderness
Muscular tenderness, spazms or fasciculations
Palpate sacroiliac joints for tenderness
Move-
- Assess active range of motion - flexion, extension, lateral flexion
-Straight leg raise / sciatic stretch test. Positive result is indicative of radiculopathy. [11]
Neurological [12]
Assess lower limb Power-
• Hip flexion/ extension/ abduction/ adduction
• Knee Flexion/ Extension
• Ankle plantarflexion / dorsiflexion/ inversion/ eversion
• Big Toe Extension
Sensation testing
• Light touch & pinprick sensation across the lower limb dermatomes – L1-S2
Rectal Examination (If trained)
Check for S3-S5 sensation (Saddle anaesthesia or paraesthesia)
Check for loss of anal tone.
Many ambulance trusts do not support internal examinations by paramedics, regardless of training and experience.
Reflexes (If trained)
Patella
Achilles / Ankle [13 , 14]
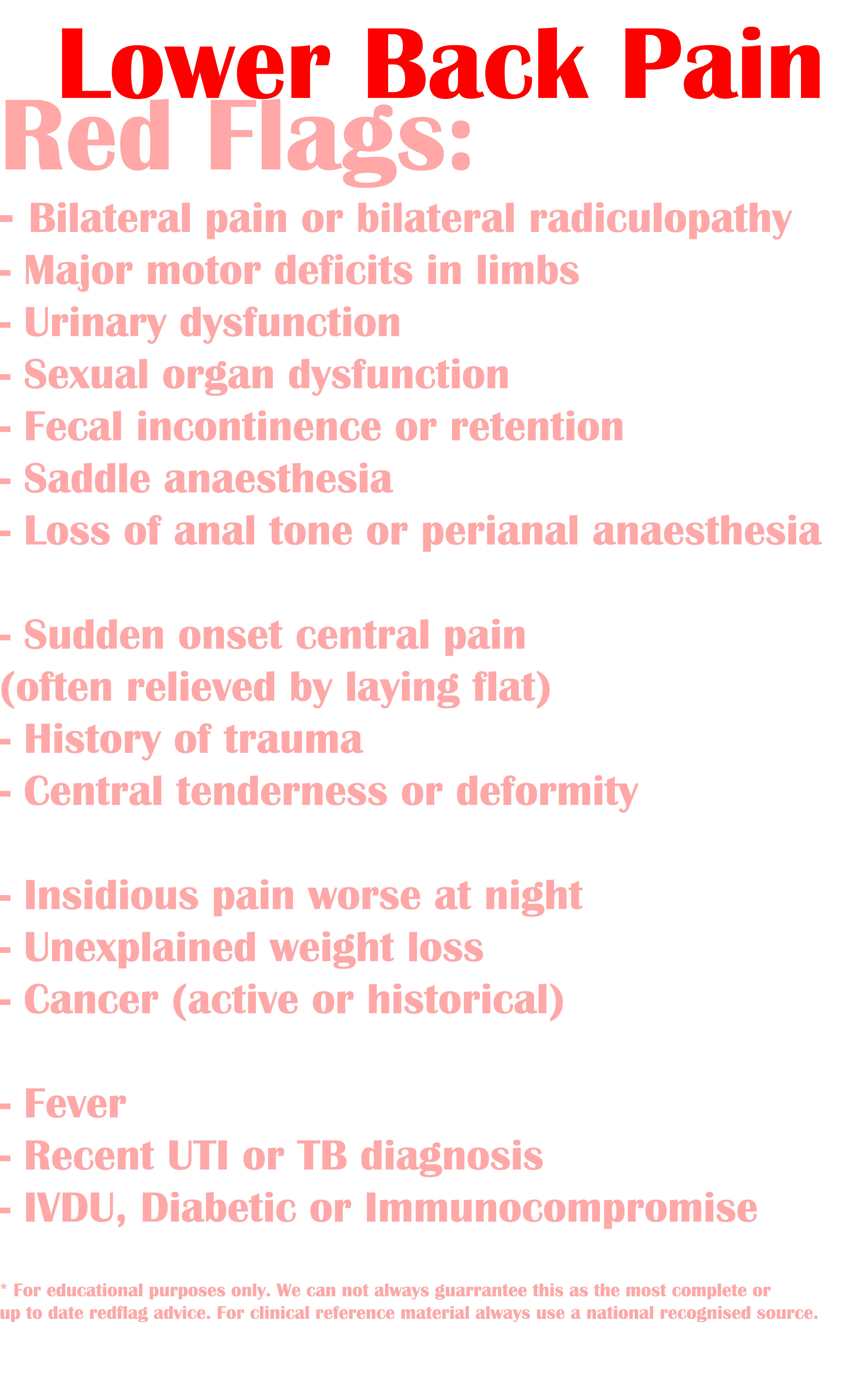
Red Flags
Whilst working through the history and examination you should pay particular attention to and screen for the following red flags that can indicate more sinister pathology and likely will require emergent or urgent referral or transport for further assessment.
Differential Diagnosis & Management-
(this list of differentials is not exhaustive)
Back Pain without radiculopathy aka mechanical/ non-specific/ simple:
History & Examination:
- Most common cause of lower back pain.
- Localised to the muscles of the lower back
- No red flag symptoms in hx or exam
- Diagnose by excluding other serious causes
Management:
- Reassure patient, explain why imaging is not needed
- Advice on using regular analgesia paracetamol QDS better taken regularly as gives better analgesic effect +/- NSAIDS if appropriate. Avoid opiates unless really necessary and then in short duration only. Consider referral to GP for ongoing analgesic needs.
- In nearly all cases does not require transport. ED will add little to this patient presentation. Analgesia can be established via primary/ urgent care pathways. Most ED management will be the same, to get some pain relief and the discharge.
- Encourage the patient to mobilise regularly. They should return to work when they feel they can.
- Give the patient specific written advice which includes likely duration, dos and don’ts of self care, advice for ongoing back care and most importantly worsening advice about red flag symptoms. It is not acceptable to write in notes ‘any concerns call 999 or if you things change call 999 or 999 SOS’. Your advice should be specific. Failure to document a thorough exam, absence of red flags and specific worsening advice is a fatal medicolegal error that can be avoided by comprehensive documentation. [5,17, 18]
Back Pain with radiculopathy/ Sciatica
History & Examination :
- Lower back pain with symptoms such as numbness, weakness or pain radiating to the buttock and leg especially if the pain radiates beyond the knee.
- Positive Sciatic stretch test
- Normally unilateral – bilateral lower limb symptoms should be considered a red flag.
Management:
- Normally can be managed by ambulance clinician using analgesia as per back pain without radiculopathy. May need stronger analgesia from primary care.
- Care should be taken to rule out more sinister forms of cord compression such as cauda equina.
- Should be referred back to the GP so that they can decide on whether further referral is needed, but in the main this is not warranted urgently.
- As above discharge with specific written worsening advice and document in notes thoroughly. [5,17]
Vertebral Fracture /Trauma
History & Examination:
-MOI indicative of possible fracture. Be wary in the elderly, long term steroid users or those with Osteoporosis who may have a lower threshold for developing a fracture.
-Spinal tenderness in the midline.
-Be aware of possibility of wedge fractures in the elderly even without trauma.
Management:
-Suspicion for fracture warrants imaging and therefore hospital transport.
-Consider if there is a need for immobilisation based upon current evidence and guidelines.
-Provide analgesia
-If major trauma suspected based upon assessment, bypass to MTC with pre alert. [19]
Cauda Equina Syndrome (CES) / Incomplete CES
History & Examination:
-Back pain + red flag symptoms of CES
-Saddle anaesthesia / paraesthesia / perianal or perineal sensory changes even subjectively.
-Bladder or bowel dysfunction or early symptoms of such as less sensation when voiding for example as per red flag section
-Bilateral sciatica/ radiculopathy or bilateral neurological symptoms found on neuro examination
-Loss of sexual function
-Many authors now discuss that when these symptoms are well established then damage has already been done and could be irreversible therefore its essential to look for early signs where management may benefit the patient. -Take patients reports of these even subjectively seriously. [20]
Management:
- Any suspicion of CES or ICES mandates emergent transport to an ED for imaging. The imaging of choice is MRI and then referral onto neuro service for definitive care. Paramedics priority must be recognition, analgesia and rapid transport. [21, 22] CLICK HERE TO READ: Journal of Paramedic Practice Article on CES (Nellist 2014)
Other Spinal Cord Compression
History & Examination :
CES is a form of spinal cord compression due to intervertebral disc herniation as the main cause. However we also need to be aware of other causes including haematoma from trauma, vertebral compression fracture, vertebral infection or primary or metastatic spinal malignancy
Be aware of insidious onset over time of these symptoms. In the patient with chronic spine problems/ degenerative spinal changes, do not pass off their symptoms of progression even if subtle.
Management:
As per CES, analgesia, rapid transport. If infection and septic manage as per sepsis.
In malignant spinal cord compression due to cancer, even in the presence of palliative metastatic disease, spinal cord compression is still an emergency that needs hospital management for treatment. The only exception to this would be someone in the absolute final days of life. However even with weeks to months prognosis steroids for symptom control would be considered. [23]
Vertebral Malignancy
History & Examination:
- Insidious onset
- Progressive symptoms over time
- Unremitting pain that is not relieved by lying or at night,
- Night sweats, weight loss, anorexia, cachexia, previous or active hx of primary CA in another location.
- Lower limb neurological symptoms
- Evidence of malignant spinal cord compression
Management:
- In the presence of symptoms of spinal cord compression, immediate transport to hospital [24]
- Otherwise urgent referral either via ED or GP for 2 week wait investigation.
Vertebral Infection/ Discitis/ Epidural Abscess/ Osteomyelitis
History & Examination:
- Common names for vertebral infection of various types however from the pre hospital perspective symptoms overlap
- Fever, central bony spinal tenderness often without hx of trauma, severe unremitting pain that doesn’t ease when lying, possibility of sepsis markers.
- IVDU/ immunosuppression / long term steroid use history.
- As above if causing compression neurological symptoms may also be present
Management:
If signs of sepsis treat as per sepsis treatment
Transport to hospital with fluids and analgesia. [25]
Acute Pyelonephritis
History & Examination:
-Fever, flank pain and vomiting are the cardinal triad of symptoms for acute pyelonephritis.
-Observe for signs of sepsis and systemic compromise
Management:
- If systemically unwell, not able to keep down meds/ fluids or has risk of developing complications such as pregnancy, immunocompromised, structural GU abnormalities, diabetes mellitus or single kidney admit to hospital.
- ED is the standard choice however as alternative pathways develop consideration can be given to ambulatory care services for medicines if these services exist locally. An approved pathway isn’t always needed just a phone call with the medical on call.
-If not systemically unwell – discuss with senior primary care clinician or GP about managing the patient in the community with oral antibiotics. They should be reviewed within 48 hours of starting antibiotics by primary care as follow up. Stringent worsening advice should be given and documented to call back if symptoms of urosepsis or deterioration develops. [26]
Renal Colic /Kidney Stones
History & Examination:
- Flank pain often radiating into iiliac fossa regions of abdomen, labia in women or testicles in men. (Consider risk of testicular tortion, do not miss this emergency condition)
- Rapid onset, pain often described as constant, patient likely to be rocking around not able to find comfortable position.
-Severe pain +++.
- Non visible haematuria on urine dip often present.
- Vomiting may be present, likely due to pain.
- May be potentiated due to dehydration [27]
- Diagnosing new renal colic in a patient over the age of 50 is risky as it can present similar to AAA rupture, have a low threshold for referring to ED for imaging to exclude aortic pathology before making this diagnosis.
Management:
If the following criteria can be met then management out of hospital is possible:
- Clinician happy with the diagnosis of renal colic
- Patient is under 50 (due to risk of misdiagnosis of aortic pathology)
- No risk factors for complications e.g. single kidney, signs of infection, renal impairment
- Pain is adequately controlled.
- Good analgesic regime can be difficult. If no vomiting consideration for oral paracetamol, ibuprofen and oromorph in combination is likely to work well.
- If you have access to specialist paramedic/ extended scope care and patient does not have contraindications IM or PR Diclofenac is a good option too.
- IV paracetamol + IV morphine could be considered for the transported patient who doesn’t respond to pain control.
- If discharging strong worsening advice is needed that if the pain returns, new vomiting or new symptoms to call 999. They should always be referred to primary care for follow up, further analgesia and the need for referral to urology as an outpatient for urgent CTKUB or USS to confirm diagnosis and exclude hydronephrosis.
- If the patient cannot be managed outside of hospital transport to ED or if locally available pathway exists ambulatory care clinic via surgical team. [27]
Abdominal Aortic Aneurysm (AAA) Pathology : Rupture or Dissection
History & Examination:
- Ripping/ tearing pain of relatively sudden onset and severe.
- Shocked/ collapsed patient
- Pulse deficits, lower limb neurology or vascular changes e.g. pallor/ mottling of lower limbs.
- Abdominal tenderness/ pulsating masses (not visible in those with large BMI and the absence of which on exam should not reassure you about the absence of the condition)
- Be aware of older adults with a first presentation of flank pain that is renal colic sounding.
- Patients who are shocked/ collapsed with new severe back pain should be considered to be aortic pathology until proven otherwise.
Management:
- Large bore IV access however consider permissive hypotension for these patients during transfer. We would likely Titrate to central pulses and GCS
- Critical care/ HEMS support if available. Helicopter transport is often useful in these patients as long distances of transfer may be needed. The reasoning for this is because you should be taking these patients to definitive care which may not be the nearest ED and needs to be a vascular surgical facility. Bypassing the nearest hospital for vascular surgery will save lives. [29]
- Consider your time lines. Activating your HEMS unit when you are in the ambulance ready to go, may not convey a time benefit to your patinet. Consider point to point conversation with your HEMS team, who will be able to offer an estimate of their own time line (considering weather, takeoff and landing times etc).
- Pre alert vascular centre with as much time as possible to prepare to receive patient. They may need to call in on call vascular surgical team.
As we mentioned in the podcast, you can find the extra case studies discussion below. Remember, clinicians are responsible for their own practice. These podcasts are produced for informative purposes and should not be considered solely sufficient to adjust practice. See "The Legal Bit" for more info.
If you’ve got any comments on the article please email generalbroadcastpodcast@outlook.com or post in the comments section.
Don’t forget to tweet and share GB if you like us using #FOAMed. If you like the podcast please leave us a review on the App store as it really helps boost our visibilty so others can find our CPD.
References :
1 https://patient.info/doctor/low-back-pain-and-sciatica
2 https://cks.nice.org.uk/back-pain-low-without-radiculopathy
4 https://www.physio-pedia.com/Referred_Pain
7 https://www.ncbi.nlm.nih.gov/pubmed/25989342
8 https://emj.bmj.com/content/35/9/556.full
9 https://www.orthobullets.com/spine/2065/cauda-equina-syndrome
10 https://geekymedics.com/spine-examination/
11 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD007431.pub2/full
12 https://geekymedics.com/lower-limb-neurological-examination/
13 https://www.uptodate.com/contents/evaluation-of-low-back-pain-in-adults
14 https://www.rcemlearning.co.uk/reference/lower-back-pain/
15 https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008686.pub2/full
16 https://bestpractice.bmj.com/topics/en-gb/778
17 https://www.nhs.uk/conditions/back-pain/
18 https://www.ncbi.nlm.nih.gov/pubmed/21214357?dopt=Abstract
22 https://www.orthobullets.com/spine/2065/cauda-equina-syndrome
23 https://www.medicinejournal.co.uk/article/S1357-3039(19)30254-3/fulltext
25 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5807463/
26 https://cks.nice.org.uk/pyelonephritis-acute#!scenario
27 https://cks.nice.org.uk/topics/renal-or-ureteric-colic-acute/
29 https://www.nice.org.uk/guidance/ng156/chapter/Recommendations#improving-surgical-outcomes