COPD Pt 1: History and Assessment
“Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable and treatable disease that is characterised by persistent respiratory symptoms and airflow limitation that is due to airway and/ or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.”
Epidemiology:
Estimated 65 million moderate -severe COPD world wide [1]
Estimated 3 million in UK….. But only 1.2 million of those have a formal diagnosis.
It’s the 5th leading cause of death in the UK
Statistics about COPD vary slightly dependant on the organisation providing them.
Causes:
COPD is caused by exposure to noxious substances, the leasing cause of this is smoking, with some sources stating it accounts for 90% of COPD cases. It’s important to bear in mind however that there are other causes, including occupational exposure.
Pathophysiology:
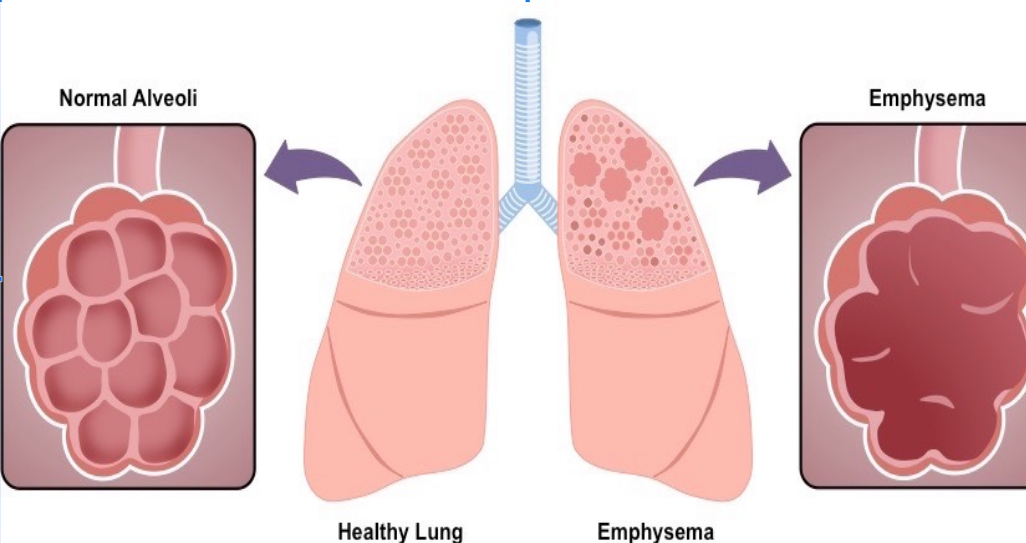
COPD is an umbrella term for 2 main conditions. Chronic Bronchitis and Emphysema. Patients will have features of both diseases but can trend more toward one or the other.
Chronic Bronchitis
Chronic bronchitis is a mucous hypersecretion problem.
Noxious particles – result in overproduction of mucous from mucous glands and goblet cells.
Over time mucous glands and goblet cells undergo hypertrophy (enlargen) and hyperplasia (increased number of) as a result, producing further excess mucous.
There is infiltration of macrophages, neutrophils and leukocytes (white blood cells) as part of the inflammatory response to noxious particles, causing inflammation of the airway lining and constriction of the smooth muscle.
Combining this results in reduced lumin space for air movement along with mucous plugging.
The airway is lined with cilia (small hairs) and a thin layer of mucous in the normal airway. The mucous is there to trap pathogens and unwanted particles and then with the cilia they beat these rhythmically back up the airway and out to be swallowed or coughed up.
However in Chronic Bronchitis the excess mucous production cause the cilia to be damaged and we loose this function.
Inspiration & oxygenation - Inflamed airway along with excess mucous results in reduced ventilation and therefore less oxygen reaching the alveoli = hypoxemia = low sats and possibly a cyanosis is o2 levels decrease significantly
Carbon dioxide retention - During expiration our distal smaller airways narrow further… in a normal airway this isn’t a problem as there is still plenty of room but in someone with CB, this results in extremely poor ventilation…..
This obstruction of the airway causes air to become trapped in the alveoli
The air that is trapped has a high paco2, this reduces the co2 concentration gradient between the alveoli and the pulmonary capillaries, resulting in less co2 moving across the respiratory membrane and being ventilated out and therefore building up in the blood resulting in hypercapnia.
Due to how narrow this airway is during expiration… the mucous in places can stick together… when we then inhale again the airway widens and the fine inspiratory crackles we can hear on auscultation is this airway re opening….. Where as wheeze is causes by the turbulent air flow through the narrowed lumen.
Credit: @rishimd twitter
Emphysema:
Normal immune response involves having a small amount of alveolar macrophages in the lungs, that are ready to respond to invading substnaces.
Smoke in this case is consumed by these alveolar macrophages in a process called phagocytosis
As part of this process they release cytokines which are signalling molecules that attract further macrophages and neutrophils to the area, resulting in inflammation.
Neutrophils produce proteases which are enzymes that break down proteins… specifically the one we care concerned with in empysema is neutrophil elastase….
Elastase breaks down elastin by hydrolysis. If You have done the anatomy and physiology pre learning you will have seen that elastin is present in both the lining of the alveoli and small airways and they are involved in the passive recoil of the chest wall during expiration and also keep the respiratory bronchioles open during expiration.
In normal healthy lung…. Compliance (ease of expanasion) and elastic recoil are equal.
With the breakdown of elastase the lungs can expand easily (increased compliance) but recoil is impaired meaning air is not ventilated out, resulting in air trapping and hyperinflation and a barrell chest appearance and hyperresonance when we percuss.
This is compounded by breakdown of elastin holding the airways open.
So In a normal airway the elastin allows recoil but holds the airways open against high pressure. When this is broken down, the airways have no counter pressure holding them open so they collapse.
This means even more air is trapped. Resulting in less oxygen getting in to perfuse the blood and less CO2 being ventilated out, again resulting in hypercapnia.
Because of the airway collapse….. Emphysema patients puff which is trying to utilise accessory muscles to force air out to increase the pressure and open the airways.
So expiration goes from being a passive process to a more active one…. As a result they use a lot more energy in the form of working the muscles of respiration including accessory muscles. As a result of this increased energy use they lose weight and often get a cachectic appearance.
So where as normally we have a nice capillary network that has a large surface area…. When the walls of aveoli get broken down and it all becomes one massive area we would have much less surface area for gaseous exchange to occur….. So this worsens perfusion.
Exacerbation of COPD:
History:
Symptoms that are typically associated with respiratory disease include:
Dyspnoea: shortness of breath associated with a wide range of respiratory pathology including pneumonia, asthma and chronic obstructive pulmonary disease (COPD).
Cough: can be productive (e.g. pneumonia, COPD, bronchiectasis) or dry (e.g. pulmonary fibrosis, side effect of ACE inhibitors).
Haemoptysis: the coughing up of blood originating from the respiratory tract below the level of the larynx. Haemoptysis is typically associated with lung cancer but can be a rare clinical feature of pulmonary embolism.
Wheeze: a continuous, coarse, whistling sound produced in the respiratory airways during breathing. It is commonly associated with conditions such as asthma, COPD and anaphylaxis.
Chest pain: typically worsened by deep inspiration due to being pleuritic in nature (e.g. pulmonary embolism, pleurisy).
Systemic symptoms: these can include fatigue (e.g. lung cancer, COPD), fever (e.g. pneumonia), and weight loss (e.g. end-stage COPD, lung cancer).
PMH – Diagnosed COPD – previous hospital admissions, frequency of exacerbations. Need for NIV/ ITU admission, asthma, heart failure, IHD.
MEDS – steroids use how often, inhalers increased use. Are they on home oxygen. Are they using nebulisers.
SOCIAL HX – Smoking, mobility, support at home, ADL management.
“Chest pain and Haemoptysis are uncommon symptoms in COPD.
If your patient has these... Consider other differentials. ”
Examination:
General - Hands may have evidence of nicotine staining, peripheral cyanosis (hypoxia or poor perphusion), palmer erythma (sign of systemic disease, can be benign), or asterixis ( this is a sign of CO2 retention, not to be confused with a fine tremor which can be from another pathology, or recent salbuatmol use). Clubbing is not a normal finding in COPD.
Respiratory - poor chest expnasion likely particularly in exacerbation, global wheeze likely, fine crackles can be COPD course basal crackles likely infective cause. Absent air entry can be sign of severe COPD meaning no airmovement or Pneumothorax. Sputum production normal in COPD, increased ammounts, increased purulence or yellow/green = likely infection.
Circulatory - Increased JVP likely, can be due ot increased pressure in the chest or CHF or likely a combination of both.
ECG changes in COPD are non specific –
Lung hyperexpansion causes external compression of the heart and lowering of the diaphragms, with consequent elongation and vertical orientation of the heart.
Due to its fixed attachments to the great vessels, the heart undergoes clockwise rotation in the transverse plane (horizontal), with movement of the right ventricle anteriorly and displacement of the left ventricle posteriorly.
The presence of increased air between the heart and recording electrodes has a dampening effect, leading to reduced amplitude of the QRS complexes.
On ECG this shows as
P pulmonale – which is large P waves due to right ventricular hypertrophy as we discussed earlier due to pressure back flow caused by corpulmonale…
Right axis deviation (I + AVF)
Low QRS voltage in the I, AVL, V5 and V6.
Sinus tachycardia may be present due to hypoxia, bronchodilator therapy or distress of the patient.
DO NOT FORGET TO CONSIDER OTHER PATHOLOGIES PRESENTED ON AN ECG. MI OR PE ARE DIFFERENTIALS TO EXACERBATION.
The second part of our podcast is out now, so be sure to check it out on Spotify or the podcatcher of your choice. The Part 2 article will be released soon!
Remember, clinicians are responsible for their own practice. These podcasts are produced for informative purposes and should not be considered solely sufficient to adjust practice. We provide lots of learning resources, so don’t just take our word for it…navigate to these and reflect on this topic further. See "The Legal Bit" for more info.
If you’ve got any comments on the article or podcast, please let us know using our Contact page, comment below or talk to us on Twitter!
If you like the podcast please leave us a review on the App store as it really helps boost our visibility so others can find our content, remember to tune in next month for our next General BroadCAST and don’t forget that you can check out our Archive for more free CPD!
References:
1 - https://goldcopd.org/wp-content/uploads/2020/11/GOLD-2021-POCKET-GUIDE-v1.0-16Nov20_WMV.pdf